Non-emergent healthcare turns to telehealth during COVID-19

Is telehealth during COVID-19 the key to solving our current healthcare predicament?
In the middle of a global pandemic, it seems strange that our medical industry is in danger. It’s instinctive to assume that a health crisis would naturally lead to a surge in medical spending. But that’s not the case at all.
While emergency care centers and ICUs teeter on the edge of full capacity, non-emergent and primary care are hanging in the balance.
Since the start of the pandemic, healthcare workers have experienced pay reductions, furloughs and layoffs. Around 40% of primary care physicians in the United States have had to lay off or furlough staff.
Across the country, the effects have been more severe for some. Many primary care and non-emergent facilities have been forced to shutter their doors altogether. As recently as July 1, less than half of primary care physicians surveyed believed they had enough capital to stay open.
While some facilities and workers continue to struggle, others are forging a new path with telehealth during COVID-19, including HIPAA compliant video chat services, live chat and voice calls. But the issues and changes run much deeper than this pandemic.
The system is fundamentally flawed
The number of primary care practices (PCPs) in the United States has steadily decreased over the last decade. This is partially because PCPs are the lowest-paid doctors in the medical field.

Take customer relationships to the next level.
Even though the United States spends more on health care (per capita) than any other industrialized nation in the world, a mere six cents or less of every dollar spent goes to primary care.
The system is flawed mostly because it functions on a fee-for-service model. The doctors get paid per service performed versus a fee for serving the patient’s needs. The medical system has shifted its focus to the quantity of patients and procedures versus the quality of care because it’s the only way to be profitable.
This fee-for-service model causes a higher level of burnout for non-emergent care physicians, but it also hurts patients’ perception of primary care. The number of people seeing PCPs dropped by 30% between 2002 and 2015 – while urgent care and ER visits increased. This decline in primary care is caused by dwindling trust and a lack of affordability under the current model.
The wide-sweeping implications of a country that foregoes primary and preventative care are predictably devastating. It’s one of the many reasons the health of the US population is declining.
The bottom line? Non-emergent healthcare has been in peril for a long time, so it’s no surprise that many were underprepared to deal with COVID-19.
Despite the lack of preparedness, many experts support the theory that this unplanned event might be the change that the non-emergent care sector has long needed.
How some practices pivoted to adapt
When the virus started, people were encouraged (or mandated) to stay home to prevent the spread of the virus. For non-emergent clinicians, this was a necessary measure, but not a sustainable one.
As a result, many medical organizations across the globe adapted to ensure that their patients continued to get care, and their businesses stayed afloat. They quickly moved to virtual technology like HIPAA-compliant video conferencing for patient appointments and live chat for booking appointments.
- Mayo Clinic increased video visits by 18,000%. In addition, they used wearable devices, symptom trackers and various apps to monitor and treat patients. Cardiologist and director for Mayo Clinic’s Connected Care, Dr. Steve Ommen, said, “… remote care will be realized as a silver lining from this pandemic.”
- IU Health Physicians added one hundred physicians to its telehealth platform at the onslaught of the virus because they believed that using telehealth during COVID-19 would be critically important for patients and practitioners alike.
- ChenMed, a medical organization that primarily manages the health of seniors, moved from 2% virtual visits to 95% virtual visits at the height of the virus. Even though some of the restrictions have lifted, 70% of ChenMed’s patient care remains virtual.
- Iroa Health provides primary care for the elderly. When COVID hit, they saw their in-person visits drop to 10% of what they were pre-COVID. They also shifted to virtual visits, because telehealth during COVID-19 may be the only way for their patients to continue to get care. In some cases, they send employees with tablets to patients’ homes to ensure that they receive adequate virtual care.
These examples are just a few of the many non-emergent physicians who have used telehealth during COVID-19 to keep up with their patients’ needs. Between March 2 and April 14, non-urgent virtual visits in the US increased by 4,345%. Approximately 97% of practices reported that they were expanding telehealth access during the pandemic.
But has this shift to telemedicine helped providers, and will it continue post-COVID?
The role of telehealth during COVID-19
Today, even as restrictions are lifted, fewer than 20% of non-emergency visits are happening in the office. The CDC is still advocating for practitioners to use telehealth during COVID-19 whenever possible.
While some medical professionals have struggled with the transition, telemedicine has been critical for keeping others’ doors open, and their patients served. NYU Langone Health scaled up its Virtual Urgent Care program and, as a result, experienced a 10-fold patient volume increase.
President of LUGPA and board-certified urologist, Richard Harris, MD, said, “If there is anything that can be said as a positive which has come out of this nightmare, it’s that we have been able to utilize telemedicine which was not available to the masses in the past… I’m not the savviest IT person in the world, and I’ve been utilizing it. It’s very simple to get engaged.”
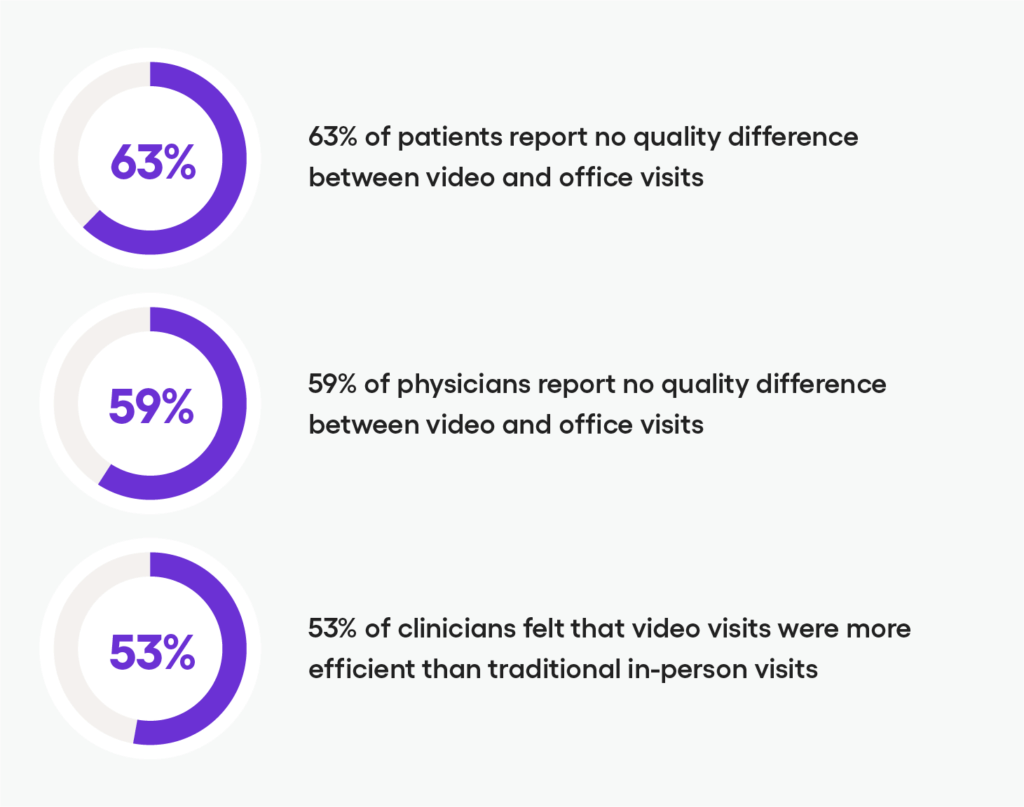
Patients and physicians mostly agree that video visits and telemedicine have been positive and comparable to face-to-face visits. 63% of patients and 59% of physicians report no quality difference between video visits and office visits.
More revolutionarily, 53% of clinicians surveyed felt that visits via video chat services were more efficient than the traditional face-to-face appointments. If we go back and look at many of the pre-existing problems with primary and non-emergent care, telemedicine helps solve quite a few, including long wait times and excess patient paperwork.
Virtual appointments are more efficient and generally result in higher-quality care. The necessity of embracing telemedicine during COVID-19 has illustrated that virtual visits could do more than just get us through this pandemic.
They could help improve the industry for good.
Thinking ahead: Implementing telemedicine during COVID-19 and beyond
Co-Director of the Larry A. Green Center, Rebecca Etz, Ph.D., said, “I don’t know that there is a ‘go back to normal.’ At this point, I think that healthcare in the US has been changed forever.”
In many ways, the explosion of telehealth during COVID-19 opened our eyes to what’s possible with healthcare. Many physicians and clinics have been advocating for a move from the fee-for-service model for years.
The COVID-19 pandemic has illustrated why that’s imperative, and the rapid adaptation of telehealth during COVID-19 has proven that it’s possible. In many ways, virtual visits are able to refocus the conversation on preventative medicine and quality of care, something that has long been missing among PCPs.
In the interim, non-emergent care facilities and physicians need to embrace telehealth. It’s an avenue to stay safely connected to your patients and may be the key to keeping your doors open for in-person care in the future.
What does this look like? It’s about incorporating fundamental solutions like video chat services, in-app voice calls, and messaging features to your practice to allow comprehensive virtual visits for the foreseeable future.
Sendbird offers the leading HIPAA compliant video and chat platform for telehealth currently used by industry leaders like Docplanner. We make it simple for customers to get started by handling the entire back end of the platform. Connect to our services over a simple-to-use API and integrate real-time communication services into your app with full peace of mind that these features are reliable, secure and compliant. Learn all about our Telehealth solutions here.
While we can’t predict the future, our bets are that telehealth is here to stay.










